In Canada, medical errors and hospital-acquired infections claim between a total of 30,000 and 60,000 lives annually. This, naturally and understandably, leading to an outflow of anger, sadness, and heartbreak for Canadian families everywhere: an emotional distress for cases that could be quite mostly preventable according to doctors. As it turns out, 138,000 (or one in every 18) patients admitted to a Canadian hospital in 2014-15 suffered some kind of harmful event that could potentially have been prevented, from getting the wrong drug to developing an infection. Of those 138,000 patients, about 30,000 had more than one adverse event that compromised their care.

Most people will experience at least one wrong or delayed diagnosis at some point in their lives, a blind spot in modern medicine that can have devastating consequences, says a new report that calls for urgent changes across health care. Team work is a big part of the action plan. Doctors, nurses, and other medical professional need to stay closely knit together in order to be able to efficiently provide the best possible and most accurate care.
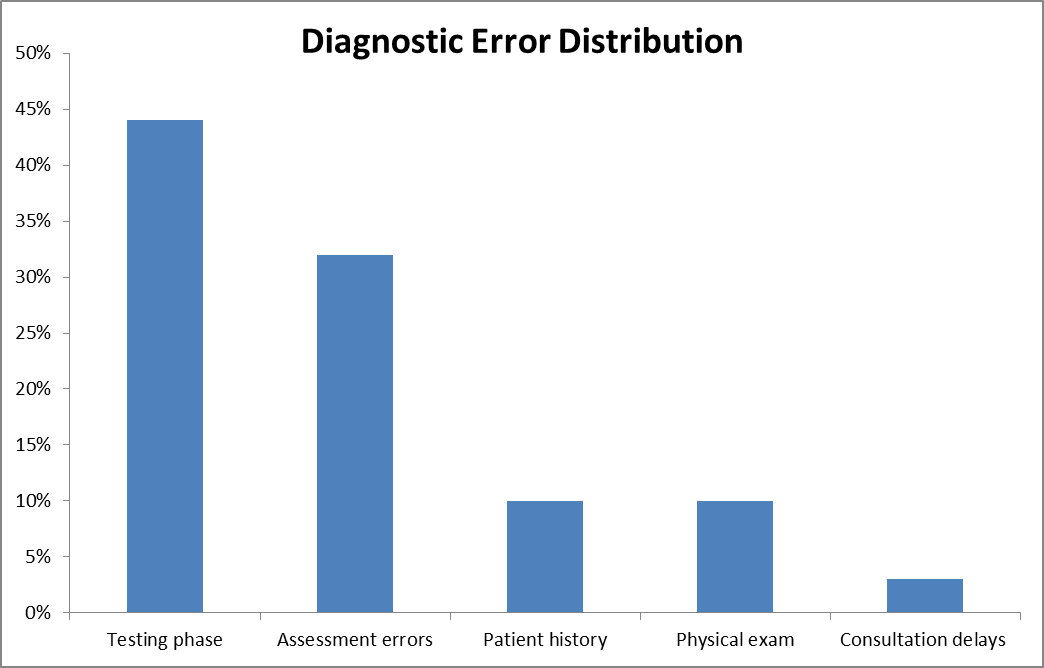
Source: https://psnet.ahrq.gov/dyk/dykdetails/63/most-diagnostic-errors-occurred-during-the-testing-phase
As exemplified by the above graph “Diagnostic Error Distribution”, it is shown that 44% of diagnostic errors generally occur in the testing phase, a period that involves reporting and follow-ups with clients. Furthermore, 32% of diagnostic errors occur due to clinical assessment errors that include actually making a mistake when diagnosing someone. According to researchers at the University of Montreal Hospital Research Centre (CRCHUM), about 20% of people getting treatment for hypertension don’t actually have it, and it’s mainly due to improperly measured blood pressure with older instruments. Continually, 20% of diagnostic errors are evenly split between mistakes in patient history or physical examination, with the remaining 3% deduced from consultation delays.
Semantic technology, as the phrase itself suggests, uses formal semantics to give meaning to all data that surrounds us. Moreover, in software, semantic technology encodes meanings separately from data and content files, and separately from application codes. This, thus, enables machines, as well as people, to understand, share, and reason with them at an executed time. Through semantic technology, adding, changing and implementing new relationships or interconnecting programs in a different way can be just as simple as changing the external model that these programs share.
Collectively, semantic technologies provide an abstraction layer above existing IT technologies that enables bridging and interconnection of data, content, and processes. Essentially, semantic technologies can be thought of as a new level of depth that provides far more intelligent, capable, relevant, and responsive interaction than with information technologies alone.
SemCare is a care process management IT solution used to facilitate the exchange of medical data. SemCare’s goal: to improve the flow of information between healthcare professionals, care givers, and, most certainly, patients. The solution’s use of semantic technology allows it to be a major player in encoding value-centered information and categorization in order to maintain a clear and concise schedule within a patient’s profile.
SemCare’s main implications lay within, of course, the medical field. Thus, most targets, historically speaking, have been within success with private/public medical sectors and medical IT firms. Fundamentally, this would include public hospitals, emergency centers, clinics and much more. Subsequently, SemCare’s use branches out to many members within the medical personnel umbrella. One major user being nurses; people who encounter and understand the importance of medical documentation and how it affects their lives as well as their patients’ lives every day.
As the primary communication tool between physicians and other health care providers, the medical record is key to good patient care and is paramount to continuity of care. It is also a legal document that must withstand scrutiny. In turn, good documentation in the medical record is accurate, objective and completed at the time of contact (contemporaneous). This means that complete and correct information is recorded and the information is factual.
The physician’s thought process is also demonstrated through good documentation. The symptoms, physical findings and laboratory results on which a plan of care is based should be identified so that the plan is clear and logical. Good documentation describes what information is given to the patient and the patient’s response. This includes notes about informed consent, the patient’s questions, the physician’s answers, and any information given to the patient about next steps or follow-up. Documentation needs to be legible and only recognized abbreviations should be used.
The following analytical elements make up a successful documentation tool:
What: Care/service provided
It’s important for healthcare providers to be clear and concise in their description of the care provided. Each patient contact, including the mode of contact if it is not in-person (e.g. by telephone, email, videoconference telemedicine), should be documented according to organizational policy and professional practice standards. Ultimately, by keeping a clear and detailed track of a patient’s medicinal intake during the hours of the day and their distinct interactions with different professionals, this allows one to save a lot of time.
SemCare enables professionals within the medical field to stay on time and within an organized schedule. Through this electronic platform, professionals can save all patient data on a clear and concise profile. This system encourages the notion of accuracy and productivity through maintaining a clean understanding of a patient’s information and, thus, discouraging misinformation all together. By having such a strong documentation system, this will inevitably allow medical workers to focus on tasks like improving waiting times.
Through having the individuality element of a personal profile, health workers can have a clear description of what the patient has undergone throughout the course of the day, and what medication, meals, and activities have transpired throughout that time.
Who: Care/service recipient and provider
Healthcare providers should ensure every page of the health record has the requisite patient identifier(s) to mitigate missing documentation when pages are separated from the health record. Patient identification on both sides of a double-sided form reduces the likelihood of the document being mixed up when it is photocopied, scanned, or faxed. In an electronic health record (EHR), ensure entries being made relate to the right patient.
Anyone reading the documentation should be able to clearly identify the healthcare provider who performed the assessment, procedure or activity. Healthcare providers should put a dated signature or initial and professional designation on every entry. The full names and titles of all healthcare providers should be documented on a master signature list. There may be the rare instance when it becomes necessary to record the care provided by others (e.g. during a code blue), but in general such practices are discouraged.
Many people interact with patients during the day. There might be a case where a hospitalized older woman may be in contact with a doctor for her medication intake during the day, a nurse in the afternoon for her shower, and another care professional in the evening for her supper. Through SemCare, you can keep track of all interactions through managing the patient’s profile. Here, anyone who comes in interaction with the patient can note down their interaction within the software.
When: Date and time the care or service was provided
The date and time of treatments, discussions or other provisions of care, as well as the date and time the healthcare provider records this information should be clearly documented. Timely documentation is especially important in high volume, acuity and turnover areas (e.g. obstetrics, the emergency department and intensive care unit) in order to keep members of the interdisciplinary team informed about changes in a patient’s status.
SemCare’s proficiency in time and date management allows medical professionals to take note and effectively document a patient’s schedule.
Why: Reason for which the care or service was provided
The purpose of each encounter should be included in the healthcare provider’s documentation. Documentation should explain why the healthcare provider did what they did given the clinical circumstances. SemCare’s use of semantics allows for encoding meanings separately from data and content files, and separately from application code.
As driven by semantic technology, the software’s “meaning-centered” capabilities allow it to perform tasks in auto-recognition of topics and concepts, information and meaning extraction, and categorization. This enables machines as well as people to understand, share and reason with them at execution time.
How: The patient’s response and outcomes to the care or service provided
To ensure documentation effectively tells the patient’s story, you should always document the patient’s response and outcomes to the interventions or care provided. Documenting the patient’s response and outcomes demonstrates that the care provided was monitored from an effectiveness and safety perspective.
All in all, SemCare offers a distinct and detailed care process management IT solution that facilitates and improves the flow, exchange, and distribution of medical data. The platform’s use of semantic technology allows for one to engrave meaning-based coding within the system, allowing for clearer and more precise descriptions.
Medical documentation is at the core of the care process today. As mentioned, and in obviousness, poor medical documentation doesn’t provide an up rise in care quality, and will definitely complicate elements such as time, efficiency, and productivity. With SemCare’s drive in semantic technology, the platform will allow care workers to better treat and holistically and effectively manage patient data.
Gabriel Pugliese, Peel Solutions 2018